About PD
Treatment options for PD
Parkinson’s disease poses daily challenges and once diagnosed, it is generally agreed that there is no clinical rationale to postpone symptomatic treatment in people who develop PD-related disability. In addition, it is recommended for patients to better manage their disease and maintain quality of life with proper diet, exercise, sleep and additional tools.
Today’s treatments are tailored to each person’s unique symptoms and there is no “one-size-fits-all” approach. In addition, none of the currently available treatments reverse the progression of the disease.
Most often, people start drug therapy when symptoms interfere with the ability to do what they want or need to do and conventional pharmacotherapy for motor symptom control is primarily based on dopaminergic replacement strategies. These are:
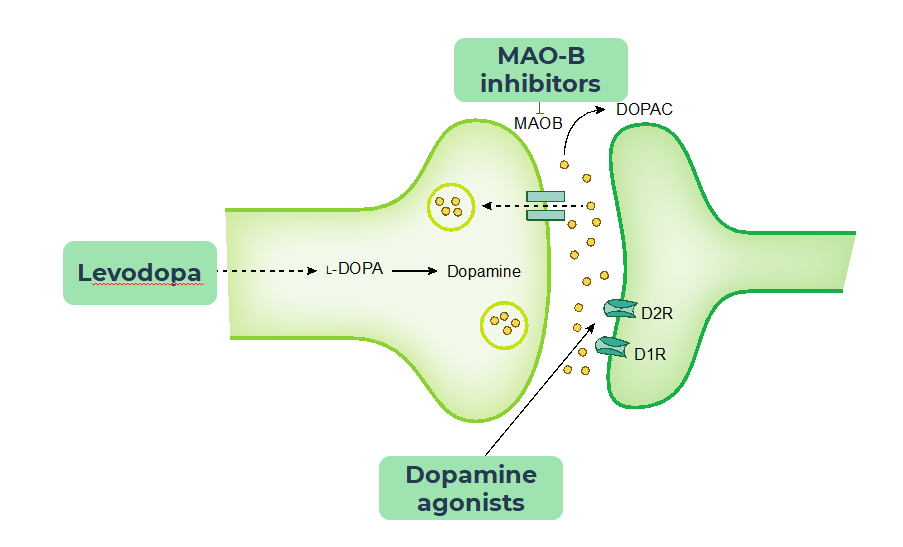
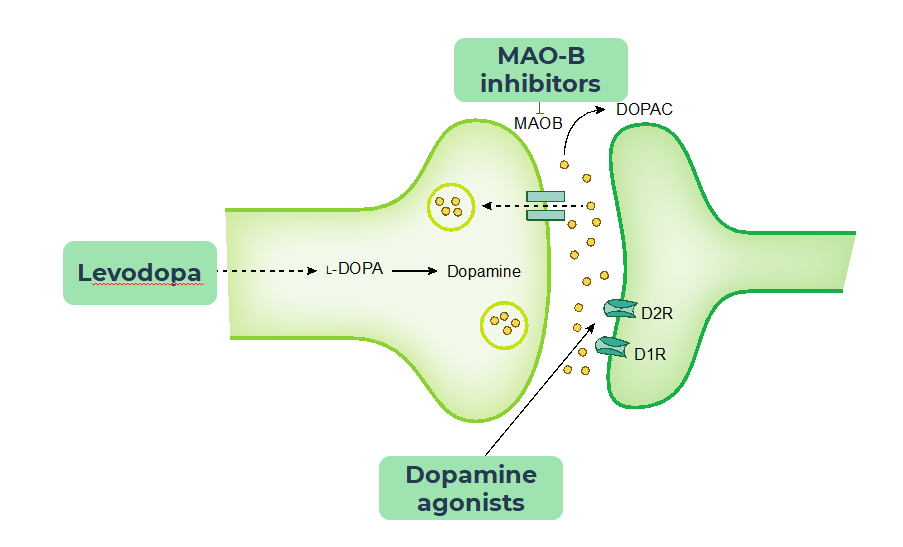
- Levodopa, considered the most effective treatment. However, chronic treatment is associated with the development of motor complications, such as fluctuations and dyskinesia, typically within 3-5 years after treatment initiation. These are dose-related. In addition, Levodopa administration requires multiple doses per day and titration is required, necessitating multiple physician visits
- Dopamine agonists, effective in relieving motor function symptoms. Side effects include excessive daytime sleepiness and a risk of sudden onset sleep episodes that can occur in unintended situations such as while driving or operating heavy machinery. Additional side effects include hallucinations, impulse control disorders, orthostatic hypotension, constipation and nausea. Titration is required, necessitating multiple physician visits.
- MAO-B inhibitors are considered better tolerated, but with limited efficacy as monotherapy. They are well tolerated with few side effects, though may lead to serotonin syndrome if concomitant medications are not monitored.